Opioid addiction, also known as opioid use disorder (OUD), is a chronic and relapsing disease that affects the body and brain. Anyone can become addicted even when opioids are prescribed by a doctor and taken as directed. Millions of Americans suffer from opioid addiction, but if you know the signs of opioid addiction to look out for you can protect yourself or someone you love from falling down a dark path. Addiction is a medical condition. Treatment can help. Recovery is possible. Read on to learn more.
What is an Opioid
You may have heard about the dramatic rise in the misuse of opioid prescription pain relievers and opioid overdose deaths. Many people misusing prescription opioids get addicted to these drugs, and the consequences are sometimes fatal. Opioids can slow down a person’s breathing; an overdose on prescription opioids can completely stop a person’s breathing. About 20,000 people die from this kind of prescription drug overdose every year in this country, and about 75 of them are teens.
Opioids, also known as opiates, are a type of drug that come from the opium poppy or are synthetically made by a drug company. Opioids can be illegal (heroin) or by prescription (painkillers). They are prescribed for pain management (OxyContin, Percocet) or addiction treatment (methadone, buprenorphine).
All opioids act the same way in the brain. Opioids are depressants, which mean that they slow down the central nervous system, including breathing.
Opioids attach to specific proteins, called opioid receptors, which are found in the brain, spinal cord, and gut. When the drugs attach to opioid receptors, they stop the body from sending pain signals to the brain. Signs of opioid addiction can stem from the critical way opioids reach with the brain creating addiction.
Signs of Opioid Addiction – What Do Opioids Do?
Opioids can cause euphoria (ecstasy), and users generally report feeling warm, drowsy, and happy. Opioids lessen stress and discomfort by creating a relaxed detachment from pain, desires, and activity. Because they are depressants, opioids also cause drowsiness, a slow heart rate, constipation, widening of blood vessels, and slowed breathing.
Opioids include:
- Heroin (dope, junk)
- OxyContin® (OCs)
- Percocet®
- Vicodin®
- Methadone
- Fentanyl
- Buprenorphine
- Morphine
- Codeine
Risk Factors for Opioid Addiction
Substance use disorders can be caused by a number of genetic, environmental, and behavioral factors. Misusing prescription medications can also lead to substance abuse or addiction. It’s important to closely adhere to prescription instructions as set by a medical professional and look for signs of opioid addiction.
Known risk factors of opioid addiction include:
- Family history of addiction or substance misuse
- Personal experience with drug use or experimentation
- Regular or heavy tobacco use
- History with mental health disorders (depression, anxiety, etc.)
- Risk-taking or thrill-seeking behavior
- Severe pressures at home or at work
- Poverty or unemployment
- Previous criminal activity
- Stressful life or family situations
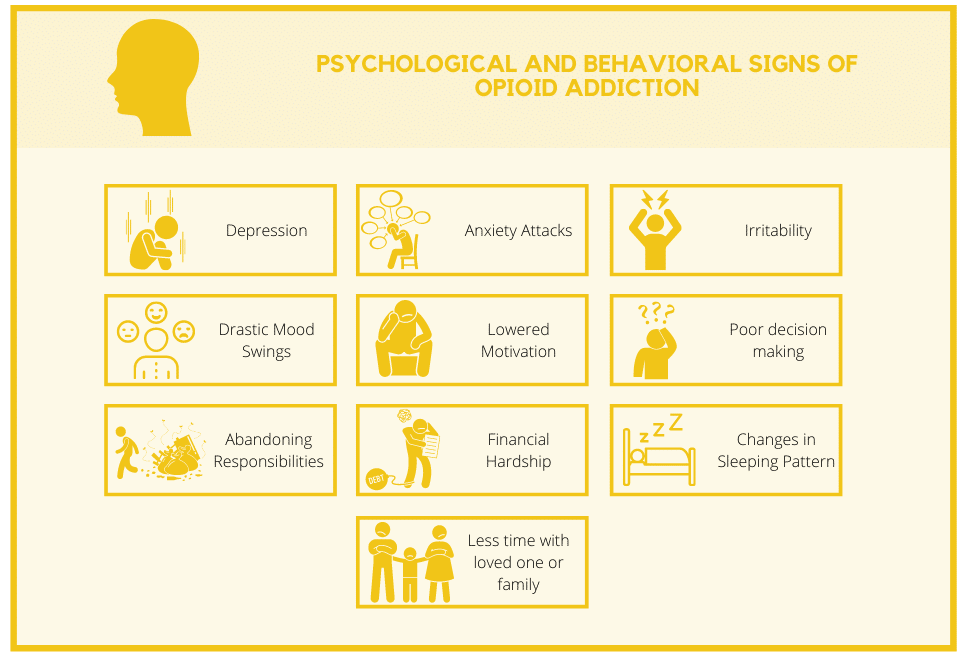
Symptoms of substance use disorders, including opioid use disorders, can be physical, psychological, or behavioral. In many cases, it can be difficult to ascertain whether someone is struggling with addiction. Potential warning signs of opioid addiction include:
Signs of Opioid Addiction
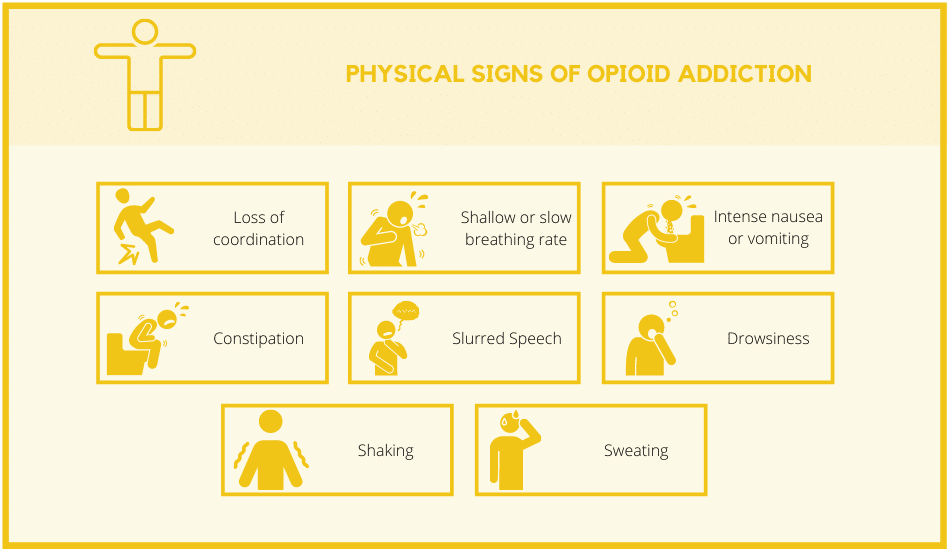
Physical
- Loss of coordination
- Shallow or slow breathing rate
- Intense nausea or vomiting
- Constipation
- Slurred speech
- Drowsiness
- Shaking
- Sweating
Psychological and Behavioral
- Depression
- Anxiety attacks
- Irritability
- Drastic mood swings
- Lowered motivation
- Poor decision making
- Abandoning responsibilities
- Financial hardship
- Changes in sleeping patterns
- Spending less time with family and loved one
Treatment for Addiction Can Help
Addiction is treatable and can be successfully managed. Treatment can help people struggling with opioid addiction get their lives back on track by allowing them to counteract addiction’s powerful effects on their brain and behavior. The overall goal of treatment is to return people to productive functioning in their family, workplace, and community. Preventing overdose death and finding treatment options are the first steps to recovery, but before that one must notice the signs of opioid addiction. While no single treatment method is right for everyone, recovery is possible, and help is available for opioid addiction.
Opioid addiction treatment:
- Helps people who are addicted stop compulsive drug seeking and use.
- Varies depending the patient’s individual needs
- Occurs in a variety of settings, takes many different forms, and can last for varying lengths of time.
- May save a life.
As with most other chronic diseases, such as diabetes, asthma, or heart disease, treatment for drug addiction generally:
- Manages the disease, is usually not a cure.
- Should be ongoing and should be adjusted based on how the patient responds.
- Needs to be reviewed often and modified to fit the patient’s changing needs.
Evidence-based approaches to treating opioid addiction include medications and combining medications with behavioral therapy. Treatment and the support and help from family, friends, co-workers, and others can make a big difference in the recovery process.
What causes opioid withdrawal?
When you take opioid medication for a long time, your body becomes desensitized to the effects. Over time, your body needs more and more of the drug to achieve the same effect. This can be very dangerous and increases your risk of accidental overdose.
Prolonged use of these drugs changes the way nerve receptors work in your brain, and these receptors become dependent upon the drug to function. If you become physically sick after you stop taking an opioid medication, it may be an indication that you’re physically dependent on the substance. Withdrawal symptoms are the body’s physical response to the absence of the drug.
Many people become dependent on these drugs in order to avoid pain or withdrawal symptoms. In some cases, people don’t even realize that they’ve become dependent. They may mistake withdrawal for symptoms of the flu or another condition.
What treatments are available for opioid withdrawal?
Opioid withdrawal can be very uncomfortable, and many people continue taking these drugs to avoid unpleasant symptoms, or they try to manage these symptoms on their own. However, medical treatment in a controlled environment can make you more comfortable and lead to a greater chance of success.
Mild withdrawal can be treated with acetaminophen (Tylenol), aspirin, or nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen. Plenty of fluids and rest are important. Medications such as loperamide (Imodium) can help with diarrhea and hydroxyzine (Vistaril, Atarax) may ease nausea.
More intense withdrawal symptoms may require hospitalization and other medications. One medication used primarily in the inpatient setting is clonidine. Clonidine can help reduce the intensity of withdrawal symptoms by 50 to 75 percent. Clonidine is especially effective at reducing:
- anxiety
- cramping
- muscle aches
- restlessness
- sweating
- tears
- runny nose
Suboxone is a combination of a milder opioid (buprenorphine) and an opioid blocker (naloxone) that does not produce many of the addictive effects of other opioids. The opioid blocker works mostly in the stomach to prevent constipation. If injected it will cause immediate withdrawal, so the combination is less likely to be abused than other formulations. When taken by mouth, this combination can be used to treat symptoms of withdrawal and can shorten the intensity and length of detoxification from other, more dangerous, opioids.
Methadone can be used for long-term maintenance therapy. It’s still a powerful opioid, but it can be reduced in a controlled manner that is less likely to produce intense withdrawal symptoms.
Need Help with the Signs of Opioid Addiction?
Seeking help for an opioid addiction will improve your overall health and reduce your risk of relapse, accidental overdose, and complications related to opioid addiction. Talk to your doctor or healthcare provider about treatment programs or support groups in your area. The overall improvement in physical and mental health is worth the pain and discomfort of withdrawal. Contact our team of medical professionals today to learn what Daylight Recovery Center can do to help you or someone you love find your way back onto the path of sobriety.



