Addiction can affect anyone regardless of race, social status, occupation, or gender. However, individuals who suffer from a mental illness are considered to be at a higher risk of struggling with addiction than those who do not. This common problem is known as a co-occurring disorder. The 2018 National Survey on Drug Use and Health determined there were nearly 9 million adults in the country that suffered from a co-occurring disorder, and the numbers are on the rise. Only 7.4 percent of these 9 million afflicted individuals ever receive the appropriate, integrated treatment their dual disorders demand.
What sets a dual diagnosis or co-occurring disorders apart from other diagnoses? Are there signs to look for in yourself or someone you love? What is the benefit of a dual diagnosis treatment, and where do you look for help? We are here to answer these common questions and more.
Q: What are Co-Occurring Disorders?
A: Co-Occurring Disorders (COD) or dual-diagnosis is a term that describes at least one psychiatric disorder and at least one substance use disorder simultaneously occurring in a person. There may be more – and this label is still very broad. As well, a co-occurring disorder can be defined as the presence of more than one addiction to a substance. Many individuals with co-occurring disorders, unfortunately, have more than one mental health issue and more than one substance-use problem which typically creates more distressing troubles.
According to one SAMHSA report, “If one of the co-occurring disorders goes untreated, both usually get worse and additional complications often arise. The combination of disorders can result in poor response to traditional treatments and increases the risk for other serious medical problems.”
Q: What are the Most Common Co-Occurring Disorders?
A: There are countless combinations of co-occurring disorders, and Daylight Recovery Center aims to address both illnesses collectively. Some conditions seem destined to come in pairs.The same sort of joining effect sometimes takes hold when an addiction is in play. In fact, it’s quite common for certain drugs of abuse to be entangled with specific mental health disorders. Here are some of the most common dual-diagnosis.
- Depression: Depression is a type of mood disorder that affects a person’s thoughts and actions. It is one of the most common mental health disorders in the U.S., and can occur in individuals of all ages, genders or backgrounds.
- Anxiety: Researchers estimate that about half of those who struggle with substance abuse experience a mood or anxiety disorder at some point in their lives. People with anxiety disorders are also two times more likely to struggle with substance abuse than the general population.
- Schizophrenia: People with either schizophrenia or schizoaffective disorder can have symptoms of depression, mania, or both types of symptoms. However, people with schizoaffective disorder tend to have more severe depressive or manic symptoms. This means that the symptoms occur more often and last for longer periods of time.
- Obsessive Compulsive Disorder (OCD): One of the most common types of anxiety disorders, OCD involves uncontrollable obsessions that trigger repeated compulsions. An estimated 24 percent of people with OCD also suffer from a substance use disorder, including alcohol abuse.
- Eating Disorders: Many of those who struggle with eating disorders have a co-occurring condition, such as anxiety, substance abuse, obsessive-compulsive disorder, depression, or post-traumatic stress disorder. All conditions should be identified and treated by someone with expertise in both eating disorders and any co-occurring conditions.
Q: Who is at the highest risk of developing a co-occuring disorder?
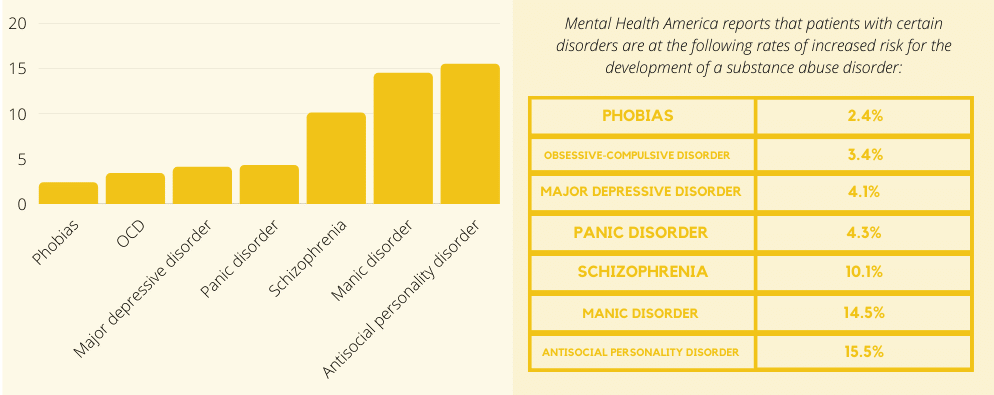
A: Mental Health America reports that patients with certain disorders are at the following rates of increased risk for the development of a substance abuse disorder:
- Antisocial personality disorder: 15.5 percent
- Manic disorder: 14.5 percent
- Schizophrenia: 10.1 percent
- Panic disorder: 4.3 percent
- Major depressive disorder: 4.1 percent
- Obsessive-compulsive disorder (OCD): 3.4 percent
- Phobias: 2.4 percent
This means that a patient who is diagnosed with antisocial personality disorder is 15.5 percent more likely than someone who is not diagnosed with any mental health disorder to also be diagnosed with a substance abuse issue.
Q: Are there Symptoms of Co-Occurring Disorders to Look For?
“It is often difficult to disentangle the overlapping symptoms of drug addiction and other mental illnesses, making diagnosis and treatment complex.”
– Nora Volkow, Director of the National Institute on Drug Abuse
A: If you believe that you or your loved one is suffering from co-occurring disorders, it is crucial to know how to recognize the warning signs. However, co-occurring disorders can sometimes be difficult to diagnose. Symptoms of substance abuse or addiction can mask symptoms of mental illness, and symptoms of mental illness can be confused with symptoms of addiction. People with mental health disorders sometimes do not address their substance use because they don’t believe it is relevant to their problems.
However, some typical patterns do emerge among those with co-occurring disorders:
- Social withdrawal: draws away from friends, family, and those who offer support
- Appetite or weight changes
- Angry, violent, or reckless behavior
- Changes in sleep patterns (insomnia or excessive sleep)
- Severe tension or worry
- Inability to concentrate
- Experiences delusions or hallucinations
- Intense or prolonged feelings of despair, hopelessness, and worthlessness
- Internal anxiety that can only be relieved by certain behaviors or rituals
- Difficulty holding a job or upholding priorities such as work or academics
- Trouble maintaining relationships because of behavior or mood swings
- Dramatic shifts in moods or energy levels
When your loved one’s problems and substance abuse become problematic for them and everyone else, it’s time to seek treatment.
Q: Are there Benefits of Dual Diagnosis Treatment?
A: The best treatment for dual diagnosis is an integrated intervention. When a person receives care for both their diagnosed mental illness and substance use disorder. The idea that “I cannot treat your depression because you are also drinking” is outdated. Current thinking requires both issues to be addressed.
No one likes to hear that they are in need of treatment. But we all need help from time to time in some way. Understanding the nature of the issues you face and what is in store for your future helps you have the power to change. When you are able to concentrate attention on all areas of the problem you are more likely to recover. One of the biggest benefits of dual diagnosis treatment is learning how to get control of the issues that currently control you. It allows you to recognize potential triggers. This helps you create a plan you can implement to avoid the possibility of a relapse.
Q: Are Co-Occurring Disorders Common?
A: Having a dual diagnosis of a mental condition and a substance addiction is not rare. In fact, many people around the country are dealing with this problem. The way that you are feeling and thinking is likely similar to the way another person is feeling and thinking. Although there is stigma that comes with mental health treatment, it is important to remember that you are not alone. Your life is unique, but as humans, many of us face the same situations in our own way.

Q: What Do You Do Next?
A: Understanding the benefits can certainly help you or your loved ones on the road to recovery. No matter how difficult or overwhelming it might be, there is always a treatment program to help you discontinue substance use and stay focused on recovery.
At Daylight Recovery Center, we have helped thousands of people suffering from CODs. The Substance Abuse and Mental Health Services Administration (SAMHSA) recommends an integrated treatment approach. Instead of treating each disorder separately without consideration for the other, we have created custom treatment programs. These programs integrate both substance abuse and mental health interventions.
Patients receive a blend of Cognitive-Behavioral Therapy (CBT) in conjunction with motivational incentives. CBT includes private and group therapy sessions, counseling, coping tools, and relapse prevention. Motivational incentives include science-based, integrative services such as massage therapy, meditation, chiropractic, auriculotherapy, and nutrition education. Our goal to treat each patient in entirety meaning treating the patient’s mind, body, and soul.
For more information about our co-occurring disorder treatment program, please call us 24/7 at [main_phone_number]. Our team of kind and compassionate medical professionals is excited to help you free yourself from the confines of addiction and mental illness and begin a fulfilling life of sobriety!



